Skin care complications from PPE: The DOs and DON’Ts
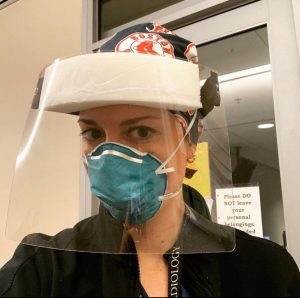 Our frontline healthcare workers are heroes who leave their homes and families to care for the ill. Besides risking infection, their work opens them to a host of other complications. They spend hours wearing personal protective equipment (PPE) to fight COVID-19, and your SkinCare Physicians’ dermatologists are now seeing skin care complications from this over video visits. Here are our recommendations to help them proactively prevent skin care issues.
Our frontline healthcare workers are heroes who leave their homes and families to care for the ill. Besides risking infection, their work opens them to a host of other complications. They spend hours wearing personal protective equipment (PPE) to fight COVID-19, and your SkinCare Physicians’ dermatologists are now seeing skin care complications from this over video visits. Here are our recommendations to help them proactively prevent skin care issues.
In general, if you’re an essential frontline worker:
- DO use a hand cream a couple times a day to counteract the irritation from frequent washing.
- DO moisturize at night to improve your skin’s barrier function.
- DON’T wear acrylic nails, false lashes or a ton of jewelry as these can be fomites.
- DON’T wear heavy make-up or foundation as these can soil your PPE, especially important if you are reusing it.
Pressure-related injuries:
Why?
The pressure from a well-fitted N95 respirator often creates indentations, sometimes even forming bruises, and occasionally breaking the skin. The indentations will fade with time, but not much can be done to prevent the pressure-related bruising.
- DO consider arnica gel patches applied at night to help the bruises resolve faster. You want to cover any open sores and wounds, as these may provide an entry point for bacterial, fungal and viral skin infections.
- DO consider Duoderm Extra Thin or a soft silicone tape under your mask to prevent and treat injuries, but check that this doesn’t compromise your mask seal. Another inexpensive, readily available option are Band-Aid Hydroseal Adhesive Bandages, which fit perfectly over the nose and malar region. Be sure to apply these to clean, dry skin, not over a cream.
- DO consider the use of barrier creams (like zinc oxide) or occlusive ointments (like Aquaphor) under your mask to increase lubrication and improve barrier function. However, these might soil your mask and face shield, so it’s best to save these for after your shift if you are routinely reusing PPE.
- DO wash the area with gentle soap and water after your shift and apply an occlusive ointment to encourage healing.
- DO consider using a headband with buttons or safety pins for your surgical mask loop if you have pressure injuries behind your ears.
- DON’T apply physical or harsh chemical exfoliants to the area as these can exacerbate any microtears in the epidermis.
- DON’T apply bacitracin or neosporin to any injuries as these predispose you to allergic contact dermatitis.

Acne:
Why?
With repeated pressure or friction on the skin, the pilosebaceous unit becomes obstructed, causing pimples. We call this “acne mechanica”, but one of our dermatologist colleagues coined the term “maskne” to describe this frustrating skin condition.
- DO gently exfoliate the areas where you are breaking out with a salicylic acid product to counteract this obstruction.
- DO consider spot treatment with La Roche Posay Effaclar Duo Acne Spot Treatment.
- DO remove any make up or sunscreen before bed.
- DON’T exfoliate harshly as this creates microtears.
- DON’T use heavy make up as this further occludes the pilosebaceous glands.
- DON’T eat large amounts of kindly donated food (e.g., pastries, pizza, and candy); such foods tend to be high glycemic index, and have been linked to acne.
Hair loss:
Why?
We predict we might soon see traction alopecia from pulling hair back tight under scrub caps and bonnets, and soon we will see hair shedding from the stress of the pandemic, or the stress of illness, referred to as telogen effluvium.
- DO keep your hair down when home.
- DO continue to eat a healthy diet.
- DO supplement with a multivitamin if your diet is lacking.
Sweating:
Why?
The gowns are plastic and induce sweating, leading to chafing. The sweating and occlusion is a set up for “heat rash” or miliaria.
- DO shower and change into loose-fitting clothing after your shift.
- DO consider a cooling anti-itch lotion like Sarna.
- DO contact your dermatologist for an in-depth video analysis and a topical steroid prescription.
- DON’T wear Spandex or tight underwear under your PPE.
Contact dermatitis:
Why?
You may develop irritant or allergic contact dermatitis from components of your mask or your gown, and start experiencing itching and rashes under these protective items. The culprit might be compounds created by washing scrubs in bleach, or glue or nickel from the mask.
- DO contact your dermatologist for an in-depth video analysis and a topical steroid prescription.
We are so grateful for all our frontline healthcare workers. You are all heroes. We hope these skin care recommendations are helpful.
Other helpful blogs:
How to beat hand dermatitis in times of frequent handwashing
How to care for your hands during the coronavirus crisis



Such a helpful article! Thanks for sharing!